Retinopathy refers to any damage to the retina of the eyes, which may cause vision impairment. Often it refers to a retinal vascular
Types of the damage that can occur in the retina are hypertensive retinopathy, a complication of high blood pressure (hypertension), and diabetic retinopathy, a complication of long-term diabetes. First, can lead to blockage of retinal arteries or veins, which in turn may eventually result in the loss of vision. Also. smoking and diabetes increase the risk of developing hypertensive retinopathy. Diabetic retinopathy is a deterioration of the blood vessels in the retina that usually affects both eyes. Diabetes is the most common cause in the U.S. Moreover, diabetic retinopathy is the leading cause of blindness in working-aged people. Almost all people with diabetes show signs of retinal damage after about 20 years of living with the condition. It can also be seen in premature newborns.
Causes of retinopathy
It is usually a sign of another medical condition. Although several medical conditions (sickle cell disease, lupus) can cause retinopathy, the most common causes are diabetes and hypertension.
Diabetic retinopathy
It is one of the most common complications of diabetes. Diabetes causes high blood sugar levels, which can damage blood vessels around the retina, that then leak protein and fats, forming deposits. The damaged blood vessels are also not as efficient at carrying oxygen to the retina. Diabetic retinopathy can be proliferative (growing abnormal blood vessels in the retina) or non-proliferative (not growing). However, non-proliferative retinopathy is much more common and may not require treatment. In the advanced stage, called proliferative retinopathy, new blood vessels grow, when the existing vessels close off. However, they are weak and often burst, causing bleeding, which can cause scarring and damage vision. Regular eye examinations are important to check for progression of disease from non-proliferative to proliferative stages. Diabetic retinopathy usually affects both eyes.
Hypertensive retinopathy
It is a complication of high blood pressure that usually takes many years to develop. High blood pressure damages the blood vessel walls, causing them to thicken and narrow, which then reduces the blood supply available to the retina, leading to retinal damage. Visual changes sometimes develop because of advancing of disease and may be a sign of undiagnosed or poorly controlled hypertension.
Signs and symptoms
Many people often do not have symptoms until there is irreversible damage. Therefore, symptoms are usually not painful and can include:
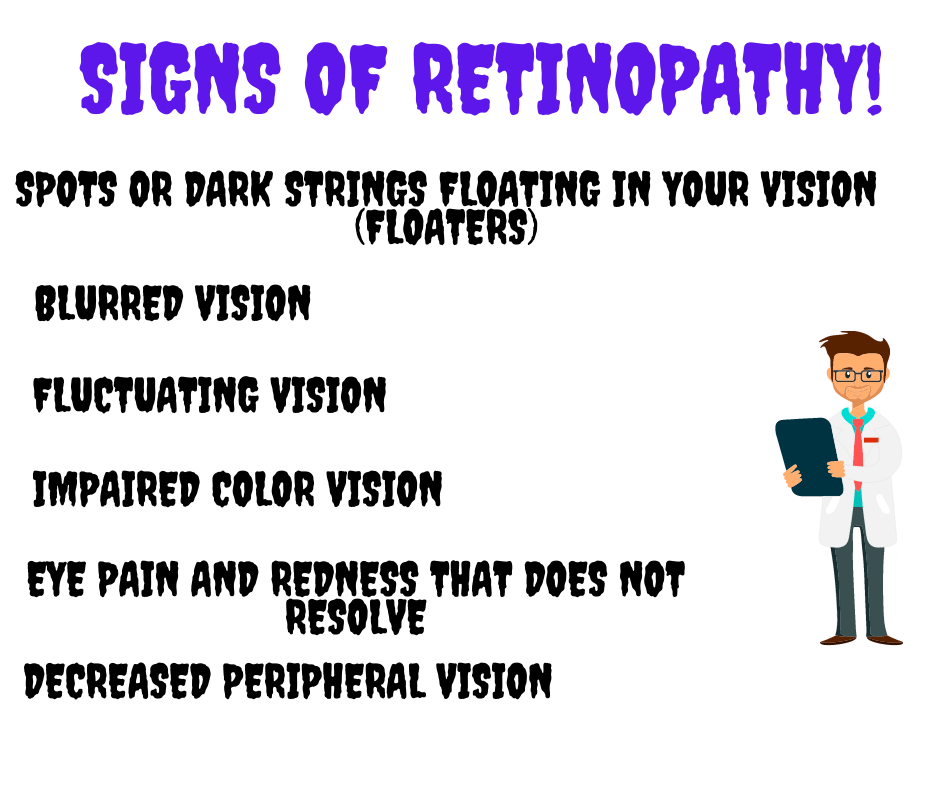
- Spots or dark strings floating in your vision (floaters)
- Blurred vision
- Fluctuating vision
- Impaired color vision
- Eye pain and redness that does not resolve
- Decreased peripheral vision
- Changes in color perception
- Headaches
The earliest sign of diabetic retinopathy that can be detected is the formation of microaneurysms. A more advanced form of diabetic retinopathy, called proliferative diabetic retinopathy, may lead to scars that decrease vision. In proliferative retinopathy, new blood vessels grow over the retina, these blood vessels may swell and burst, causing bleeding and damage to the eye.
Diagnosis and treatment
This disease is diagnosed by an ophthalmologist during a comprehensive dilated eye exam that usually includes: visual acuity testing, tonometry, pupil dilation and optical coherence tomography (OCT). If severe diabetic retinopathy is suspected, a fluorescein angiogram may be used to look for damage or leakage in blood vessels. In the case of hypertensive retinopathy, an ophthalmologist will look for tiny cholesterol plaques as well as narrowing and thickening of the blood vessels.
Managing disease
The key to treating disease is managing the underlying causes behind this condition. Moreover, controlling blood sugar levels in diabetes is critical in delaying the progression of diabetic retinopathy. Keeping blood pressure under control will help prevent hypertensive retinopathy. Regular exercise, proper diet, supplements and other lifestyle changes such as quitting smoking will reduce the risk of developing disease. Therefore, early treatment is essential to prevent blindness.
Laser treatment
Today, many retinal problems are treated with lasers. Evidence shows that laser therapy is generally safe and improves visual symptoms. If a blood vessel has already leaked and scarring has occurred, your doctor may advise you to have a vitrectomy, which involves removing a part of the vitreous humour along with the scar tissue. Treatment includes medications to control blood pressure, laser treatment, and medications injected into the eye (corticosteroids).