Cardiac tamponade, also known as pericardial tamponade, is a serious medical condition caused by the accumulation of fluid or blood in the pericardium (the sac around the heart), resulting in the reduced ventricular filling which keeps your heart from functioning properly. Because of this, your heart can`t pump enough blood to the rest of the body, which makes this condition a medical emergency. If not treated it can lead to complications such as pulmonary edema, organ failure, shock, cardiac arrest, and even death.
Cardiac tamponade is usually the result of penetration of the pericardium, which is double-walled, thin sac that surrounds the heart. Common causes of pericardial penetration or fluid accumulation might be gunshot or stab wounds, trauma to the chest from a car accident, a ruptured aortic aneurysm, cancer that has spread to the pericardial sac, accidental perforation after cardiac catheterization or angiography, pericarditis, heart attack, kidney failure, hypothyroidism and many more. Other possible causes include leukemia, radiation therapy to the chest, systemic lupus erythematosus, dermatomyositis, and heart tumors.
Symptoms and diagnosis of cardiac tamponade
Symptoms of cardiac tamponade may vary with the acuteness and underlying cause of the tamponade. Patients with acute cardiac tamponade show signs like tachycardia, dyspnea, and tachypnea. Other symptoms and signs may include: low blood pressure, weakness, chest pressure, anxiety, fainting, dizziness or even loss of consciousness, decreased urine output, trouble breathing, cold and clammy extremities.
Diagnosis
Prompt diagnosis is key to reducing the mortality risk for patients with this condition. There are often three signs any doctor can recognize, they are commonly known as Beck`s triad. They include:
- Low blood pressure and weak pulse, because of reduced blood pumping by your heart
- Extended neck veins
- A rapid heartbeat combined with muffled heart sounds, due to the increasing level of fluids in the pericardium
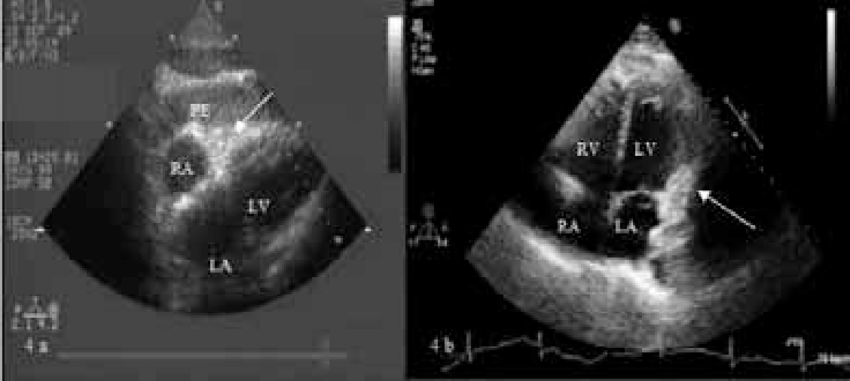
Tests that need to be done for the diagnosis are firstly echocardiogram, an ultrasound of the heart, then chest X-rays, a thoracic CT scan, a magnetic resonance angiogram, and an electrocardiogram.
Pathophysiology of cardiac tamponade
The pericardium, which is the membrane surrounding the heart is composed of 2 layers. The ticker parietal which is an outer fibrous layer and the thinner visceral which is an inner serous layer. Normally the pericardial space contains 20-50mL of fluid. During cardiac tamponade there are 3 phases of hemodynamic changes, as follows:
- Phase I – The accumulation of pericardial fluid impairs relaxation and filling of the ventricles, which leads to a higher filling pressure. At this point, the left and right ventricular filling pressures are higher than the intrapericardial pressure
- Phase II – As fluid continues to accumulate, the pericardial pressure increases above the ventricular filling pressure, this leads to resulting in reduced cardiac pressure
- Phase III – A further decrease in cardiac output occurs, which is due to the equilibration of pericardial and left ventricular filling pressures
The underlying process in the development of tamponade is a reduction in a diastolic filling, which occurs when transmural distending pressure becomes insufficient to overcome increased intrapericardial pressure. To maintain the cardiac output heart rate grows rapidly, which leads to tachycardia. Systemic venous return is also altered during cardiac tamponade because the heart is compressed due to the increased intrapericardial pressure.
Treatment of cardiac tamponade
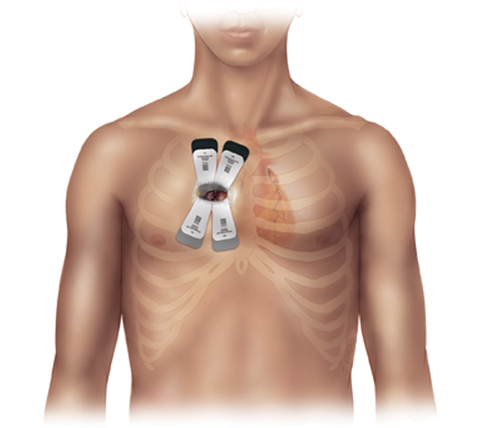
Cardiac tamponade is a medical emergency that requires urgent hospitalization and drainage of pericardial fluid. The treatment has two purposes, firstly it should relieve pressure on your heart and then treat the underlying condition. Preferably, patients should be monitored in an intensive care unit, and the doctor needs to make sure that the patient is stabilized. Initial management in the hospital is by pericardiocentesis, this is a procedure that involves the insertion of a needle through the skin and into the pericardium, and then under ultrasound guidance aspirating fluid. Almost every time, a cannula is left in place for 1-2 days, so that the procedure can be performed again if the need arises. If a patient has penetrating wound the doctor can perform a more invasive procedure called a thoracotomy to drain blood.
During hospitalization, all patients should receive: oxygen, fluids, and medications to raise blood pressure. It is strongly recommended to be rested in bed with leg elevation because that can help increase venous return. Once the tamponade is under control and the patient`s condition stabilizes, the doctor may perform additional tests to determine the underlying cause of cardiac tamponade.
The long-term outlook depends on how quickly the diagnosis was made, the underlying cause of the tamponade, and any subsequent complications. The outlook is really good if the cardiac tamponade was quickly diagnosed and treated. So it`s important to seek medical help as soon as you notice any of the signs of symptoms.
