Angiotensin-converting-enzyme inhibitors
(ACE inhibitors)
ACE inhibitors are an important group of drugs in the treatment of cardiovascular diseases, and their discovery resembles one of the most significant advances within this field of medicine. Firstly synthesized ACE inhibitor is captopril, discovered in 1975 by Ondenti, Rubin, and Cushman at US pharmaceutical company called Squibb. Historically looking, the first ACE inhibitor was found in the poison of Brazilian snake Bothrops Jararaca. Its poison is decreasing the blood pressure, and in 1968, the Nobel prize winner, John Vane proved that this venom indeed inhibits the activity of angiotensin-converting-enzyme. Since captopril causes several side effects, and it needs to be taken 2-3 times a day, many ACE inhibitors were developed.
Renin-angiotensin system
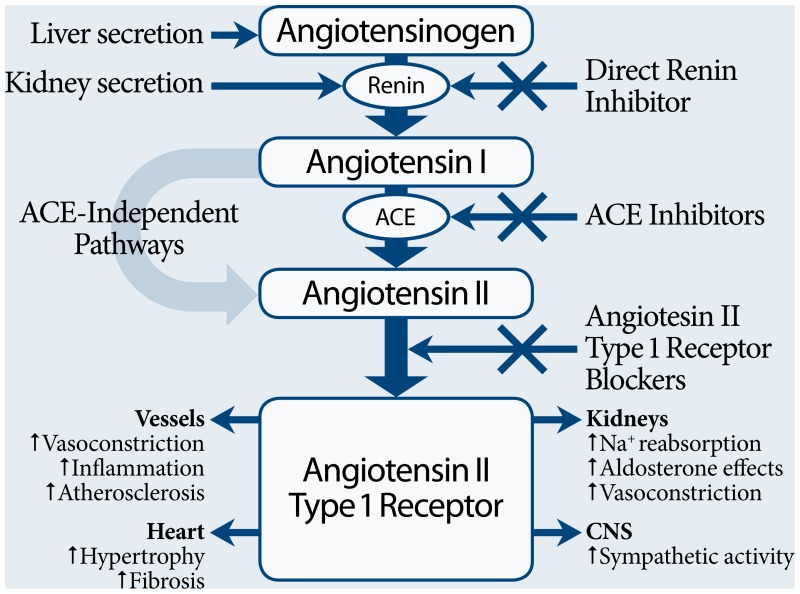
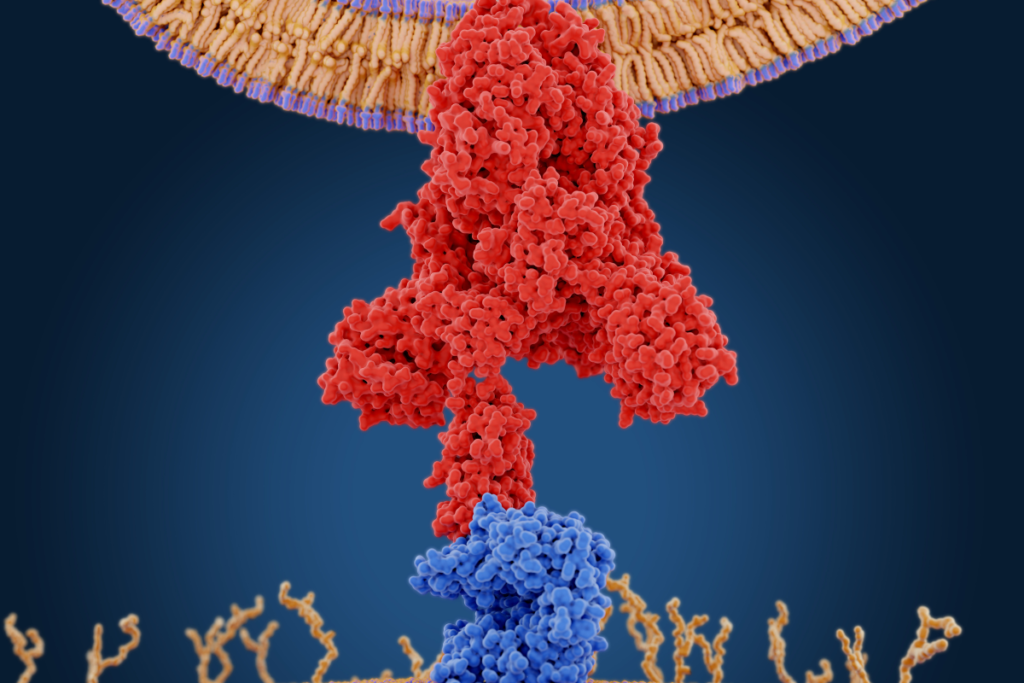
Renin-angiotensin system is a natural organism’s way to manage the blood pressure. Renin is a protein, which is released by kidneys as a response from juxtaglomerular apparatus to lowered renal perfusion pressure, lowered sodium load, or activity of sympathetic nervous system via β1 receptors. Renin acts as an enzyme. It hydrolyzes (breaks down) the angiotensinogen, produced and released by the liver, into a peptide called angiotensin I, which doesn’t have any particular biological function on its own. When angiotensin I circulate throughout the bloodstream it comes in contact with angiotensin-converting enzyme (ACE), which is predominantly localized in vascular endothelial tissue of the lungs.
ACE is converting angiotensin I into a powerful vasoconstriction agent angiotensin II, while it also induces the disintegration of bradykinin (a vasodilating agent). Angiotensin II can directly narrow down the blood vessels, and this effect is more prominent in arteries, while it’s significantly lower in veins. Vasoconstriction is elevating the blood pressure increasing the peripheral resistance. This mechanism is really important in injuries with high blood loss, as it prevents the critical lowered blood pressure which may lead to hemorrhagic (hypovolemic) shock. Angiotensin II increases the activity of the sympathetic neural system and stimulates the release of aldosterone, which is causing retention of sodium and water, increasing the blood pressure, while eliminating the potassium to maintain the neutrality of electrolytes. It also promotes cardiac remodeling, which worsens the heart function. Enzymes called angiotensinases are responsible for degradation of angiotensin II. It is known that several other enzymes can convert angiotensin I to angiotensin II.
While the renin-angiotensin system is an important mechanism of blood pressure regulation, its improper function is one of the main reasons for high blood pressure.
Types
ACE inhibitors are effective drugs for treating hypertension, and they are very alike one to another. The main difference is in chemical structural groups, and in the term of elimination from the organism via the liver or via kidneys, which is important for patients with certain conditions related to these organs. Most of them are prodrugs, meaning that they are converted into an active form within the body.
Sulfhydryl-containing agents
ACE inhibitors that have an -SH group are captopril and zofenopril. This group is responsible for an abnormal taste (metallic or salty), and lower lasting of the drug effects, but it resembles a strong ligand for Zn molecule which empowers the drug activity and vasodilation.
Dicarboxylate-containing agents
This is the largest group of ACE inhibitors, including enalapril, cilazapril, ramipril, quinapril, lisinopril, perindopril, benazepril, trandolapril, and others. They have a dicarboxylate group, which has an affinity for Zn molecule, but shows fewer side effects.
Phosphonate-containing agents
The representative of this group is fosinopril. It contains a phosphonate group with phosphorus which also shows fewer side effects than sulfhydryl containing agents.
Mechanism of action
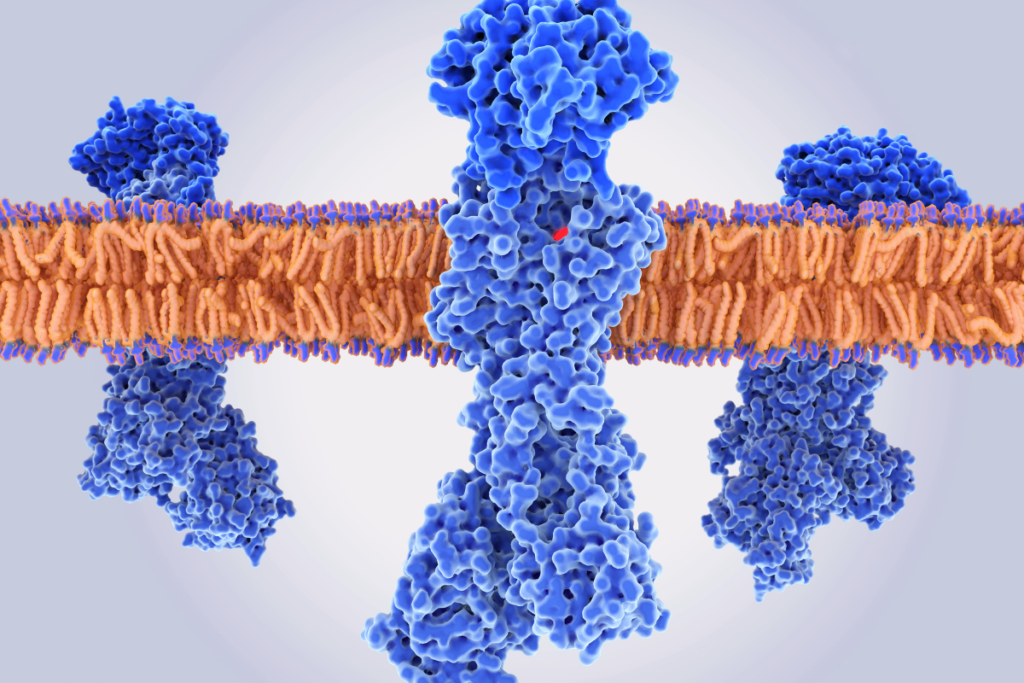
ACE inhibitors’ mechanism of action relies on blocking of angiotensin-converting enzyme, which transforms the inactive angiotensin I into potent vasoconstrictor Angiotensin II. An additional effect of these drugs is the preserving of bradykinin which acts as a vasodilator, as it is degraded by the angiotensin-converting enzyme.
Indications
While they are generally antihypertensive drugs, they are prescribed in other heart-related disorders like heart failure, and ACE inhibitors are often used in primary and secondary prevention of the heart attack. Other indications include chronic kidney disease and diabetic nephropathy.
Hypertension
Hypertension represents the blood pressure above 140 / 90 mm Hg. In most cases it is an idiopathic disease (without a known cause), frequently followed by disorders in the renin-angiotensin system. This group of drugs is first to be introduced in the therapy of newly diagnosed hypertension in people younger than 55 years. They are effective drugs and should be given in low dosage at first, increasing it over time, because they could cause hypotension. ACE inhibitors are favored in the treatment of hypertension accompanied by diabetes, kidney dysfunction, heart failure, and heart attack. They lower the blood pressure decreasing the vascular resistance, inhibiting the conversion of angiotensin I to angiotensin II, preserving the bradykinin, which widens the blood vessels. ACE inhibitors encourage sodium and water elimination, easing circulation and blood pressure.
Heart attack
A heart attack occurs when the blood vessels that supply the heart are obstructed, depriving a part of the heart of oxygen and nutrient-rich supply, which leads to the death of heart cells. One of the big problems in this condition is heart remodeling, which happens after the initial damage. Remodeling might sound good, but quite the contrary, an increase in size, shape, and function lead to a higher risk of sudden death and worsening of the heart’s function. Angiotensin II is inducing these changes, and ACE inhibitors block the transformation of angiotensin I, thus preventing the heart to change in a bad way. Cardioprotective effects come from reducing of blood pressure, preload and afterload, sympathetic nervous system activity, and prevention of heart remodeling.

Heart failure
Heart failure is a disease in which the heart can’t adequately supply the organs and peripheral tissues. ACE inhibitors lower the blood pressure; reduce the preload – the amount of ventricular stretch before contraction, during the diastole, which regulates the symptoms of pulmonary congestion, swelling of ankles, lower legs, and abdomen; reduce the afterload -the resistance that heart needs to overcome to pump the blood into the circulation, which improves its blood pumping function, and stroke volume. They are preventing cardiac remodeling and activation of the sympathetic nervous system, which additionally damages the already weakened hear, thus reducing the rate of mortality and hospital visits, prolonging life.
Chronic kidney disease
Chronic kidney disease or chronic kidney failure is a condition where the kidneys lose their function over time. Their ability to eliminate excess fluids and wastes from blood is compromised, which may lead to the dangerous build-up of unnecessary, and toxic substances in the patient’s organism in later stages. As high blood pressure is one of the most common causes of chronic kidney disease development, the use of ACE inhibitors in this condition is helpful in more than one way. Besides the lowering of blood pressure, they are acting renoprotective, they reduce proteinuria (abnormal amount of proteins in urine) and protect the function of kidneys.
Diabetic nephropathy
Diabetic nephropathy of diabetic kidney disease is one of the complications of diabetes. Approximately 30 – 40% of these patients develop it over time. The high glucose concentration in blood can damage the structure of a kidney that is responsible for blood filtration, leading to proteinuria (proteins leaking into urine). High blood sugar is causing scarring, which may lead to a life threating condition, the kidney failure (end-stage kidney disease), but in most of the people, diabetic nephropathy doesn’t progress into this. Hypertension is damaging the kidneys and it increases the risk for kidney disease. ACE inhibitors regulate high blood pressure, and with their renoprotective effects, reduce the proteinuria and protect the kidneys.
Contraindications
ACE inhibitors, like any other drug group, shouldn’t be used in certain conditions. These conditions include pregnancy, history of angioedema, bilateral renal artery stenosis or unilateral stenosis of a solitary functioning kidney, aortic stenosis, and hypotension.
Pregnancy
ACE inhibitors are teratogenic (causing developmental malformations) drugs and should be avoided completely during the pregnancy, and in women who are planning a pregnancy. This group of drugs can induce a renal dysfunction of the fetus, as well as a malformation in the cardiovascular and central nervous system.
Renal stenosis
If both arteries that supply the kidneys are narrowed, or if a patient has one functioning kidney, and its artery is narrowed, ACE inhibitors shouldn’t be used. Angiotensin II is important in this condition to keep the blood filtration because it constricts the efferent arteriole which is leading the blood out of the kidney. If ACE inhibitors are used they will widen the efferent artery disrupting the difference in pressure, and thus interfere with filtration, which may lead to renal failure.
History of angioedema
Angioedema is a swelling of the lower layer of skin which may occur particularly on the face, larynx, or tongue, but may happen in other body parts. In severe cases, this condition may cause respiratory arrest and death. ACE inhibitors shouldn’t be used in people with a history of any type of angioedema, hereditary, idiopathic, or angioedema caused by previous use of ACE inhibitors or angiotensin II receptor blockers.
Aortic stenosis
Aortic valve stenosis is a heart valve disorder which refers to narrowing of the heart’s aortic valve. Its function is disrupted. It can’t open fully and maintain the normal blood flow, and it’s blocking the blood passing into aorta and circulation. ACE inhibitors can induce dangerous hypotension because cardiac output can’t increase to compensate for the decreased vascular resistance due to the inability of the aortic valve to open.
Hypotension
Hypotension is a blood pressure lower than 90 / 60 mm Hg. ACE inhibitors are antihypertensives, and their primary function is to decrease blood pressure. If the blood pressure is reduced even lower, it could lead to a dangerous, life-threatening state of shock.
Side effects
ACE inhibitors may show some side effects in certain patients as all other medication types do, but they are not so frequent.
- hypotension – like all other antihypertensives, ACE inhibitors can lower the blood pressure, below normal levels; this mostly happens due to their combined use with other drugs with this effect (diuretics), and in people who are on sodium restricted diet
- dry cough – dry cough is the common side effect of these drugs, and it is a consequence of the accumulation of bradykinin in lungs; patients who experience this effect are often switched to use of angiotensin II receptor blockers
- angioedema – this is rare, but a dangerous side effect, which can sometimes lead to death; increase in bradykinin levels is also responsible for this effect, so if someone experienced this sort of problem, ACE inhibitors should be excluded from their therapy
- hyperkaliemia – high concentration of potassium in the blood may happen due to its blocking of aldosterone effects of preserving the sodium and elimination of the potassium; hyperkaliemia may be dangerous, as it induces dysfunction of the heart
- acute renal failure – ACE inhibitors are given to prevent renal problems in some cases, but if a patient has renal artery stenosis, they can invoke a kidney failure, as they lower glomerular filtration
- headache, dizziness, drowsiness – these may be caused due to vasodilation
- upset stomach – a possible side effect of many drugs
- abnormal taste – metallic or salty taste due to a sulfhydryl group of some ACE inhibitors
Interactions
ACE inhibitors may come in interaction with other medications, so it’s important to note to your doctor or pharmacist if you’re using them.
Potassium-sparing diuretics
Potassium-sparing diuretics are used as additional therapy in the treatment of hypertension and heart failure. They are increasing the concentration of potassium in the blood, and if they are combined with ACE inhibitors who do the same, a hyperkaliemia may occur.
NSAID
Nonsteroidal anti-inflammatory drugs can invoke an increase in potassium concentration if they are combined with ACE inhibitors in compromised kidney function. Long term usage of NSAIDs can decrease the antihypertensive effect of the ACE inhibitors.
Lithium
Lithium is mostly used for treating bipolar disorder. If it’s used during the treatment with ACE inhibitors, its concentration in blood may rise, and cause toxic effects
