Deep vein thrombosis

Epidemiology
Deep vein thrombosis is a common disease associated with higher mortality, particularly in older age. Every year about 1 in 1000 people develop this disorder. It is fairly rare in children meaning that the incidence is 1 in 100 000 a year, while the risk greatly increases after the age of 60, where the incidence is 1 in 100 people, and 1 in 10 in very old people. The incidence in the United States is approximately 300 000 – 600 000 people each year. People of Asian descent have a lower risk than Caucasians and people of African origin.
Hemostasis and thrombosis
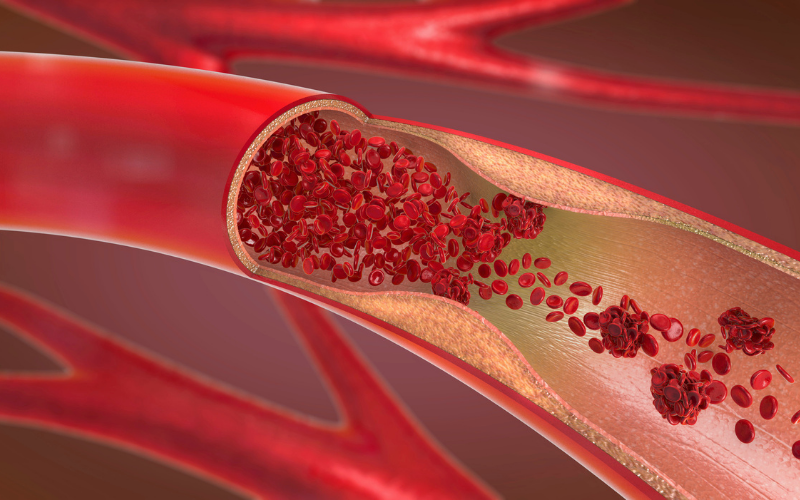
Hemostasis is a physiological process that stops the bleeding in blood vessel damage. Because the blood in blood vessels is under pressure, the laceration or rupture of the blood vessel is causing bleeding (hemorrhage). If a small blood vessel is injured, bleeding usually stops spontaneously. However, in the injuries of large arteries and veins, this process is not so effective, and those injuries should be regulated by surgical procedures. Hemostasis begins with vasoconstriction (narrowing of blood vessels), which reduces the blood flow and blood loss. Platelets adhere to the damaged blood vessel. Adhered platelets are activated, they change shape, empty their granules that stimulate further interaction between platelets, called aggregation, forming a plug.
When the platelet plug is formed, the blood coagulation happens. The coagulation factors lead to fibrin formation. Fibrin assembles a net around the plug which consolidates it making a blood clot. In the end, the blood vessel heals and blood clots are resorbed by a process called fibrinolysis.
Thrombosis is a pathological process of blood coagulation which occurs in absence of blood vessel damage. It follows the same process as hemostasis. The factors that contribute to thrombosis are described in Virchow’s triad.
- Interrupted blood flow (stasis of blood flow) – Caused by Atrial fibrillation, prolonged immobility (long car and plane journeys, hospitalization), varicose veins, obesity, or pregnancy.
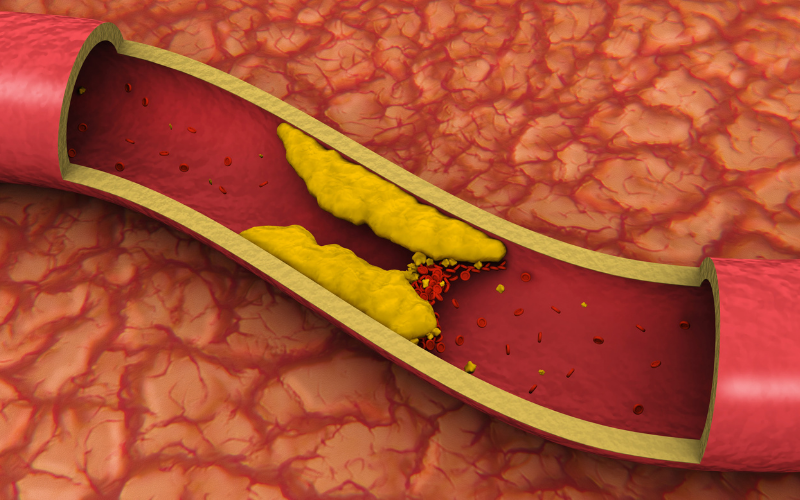
- Irritation of the vessel and its vicinity (Endothelial injury) – Caused by Hypertension, atherosclerosis, vascular catheters, and other endothelial injuries.
- Hypercoagulability – Caused by Tumors, pregnancy, hereditary thrombophilia, obesity, cigarette smoking, hormonal contraceptives, or elderly age.
Thrombosis can occur in any part of the cardiovascular system including arteries, veins or the heart.
Deep vein thrombosis
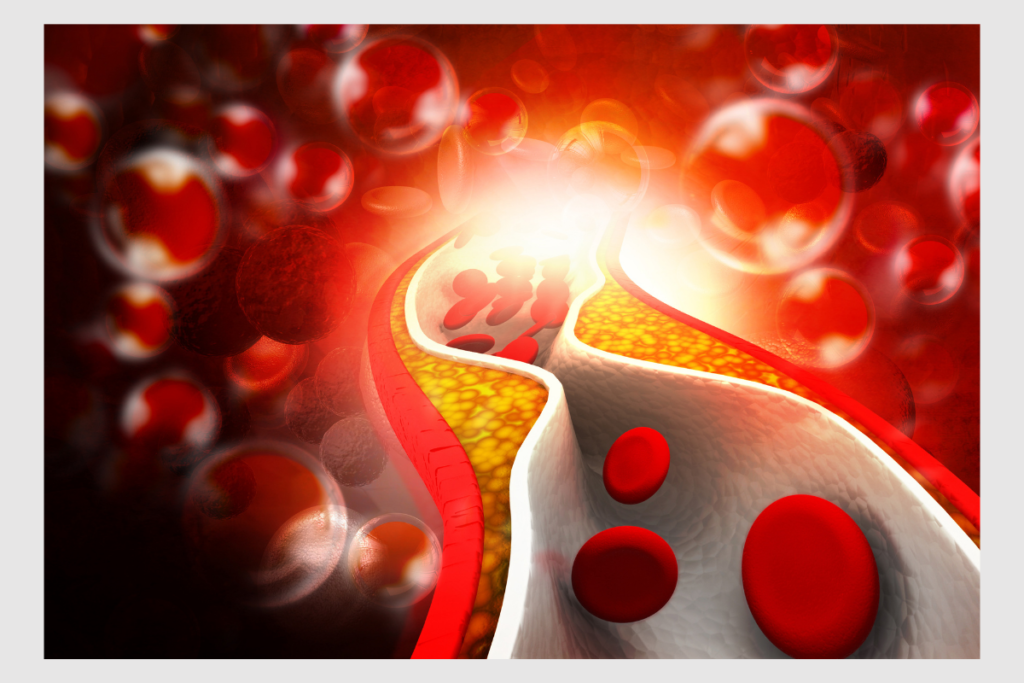
Unlike the peripheral vein thrombosis, which can heal spontaneously, the deep vein thrombosis is a more serious condition. Two factors from Virchow’s triad that are responsible for vein thrombosis are hypercoagulability and interrupted blood flow. The stasis of blood flow weakens the dilution of activated coagulation factors, thus increases the chance for blood clot forming.
Deep vein thrombosis most commonly occurs in veins of a lower leg, less commonly in the upper leg, and rarely in arms, brain, or gastrointestinal veins. The blood clot formed in veins can break loose, travel to other body parts, and then it is called an embolus. The embolus can obstruct the vessels in the lungs, inducing the pulmonary embolism, which is a life-threatening condition. Blood clots from lower leg usually don’t lead to pulmonary embolism, but if they aren’t treated, they can progress to upper leg veins, which increases the chance for pulmonary embolism greatly.
Symptoms
Deep vein thrombosis can sometimes go without any symptoms, especially if it’s localized in the lower leg, but the common ones include:
- Swelling – Usually only one leg is swollen, but sometimes there is swelling in both legs.
- Red or discolored skin – The skin near the affected area is red or discolored. Sometimes the skin looks pale and reddish.
- Pain – The pain is felt in the part near the blood clot forming. The pain may expand throughout the circulation from the place of origin.
- Difficulty walking – The pain in a leg is making it difficult to walk.
- Warmth felling -The warmth is felt in the affected area.List Item #3
- Ulceration – Ulceration is rare, but can sometimes happen in deep vein thrombosis.
Risk factors of deep vein thrombosis
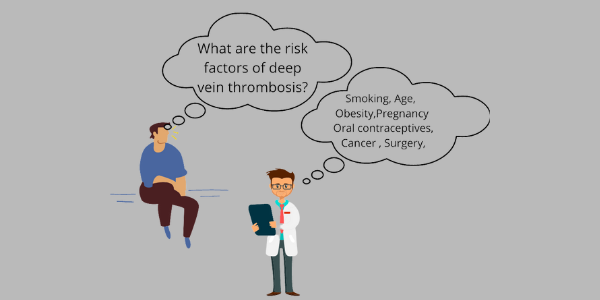
Surgery or severe trauma
Severe trauma of veins, or recent surgery may increase the chance for blood clotting.
Prolonged immobility (long car and plane journeys, prolonged bed rest in hospital stays, or paralysis)
When you don’t move for a certain amount of time, muscles in your legs don’t contract. Blood flow isn’t stimulated, and conditions for blood clot making are satisfied.
Genotype
Certain hereditary characteristics may lead to genetic disorders of increased thrombocytes production and increased coagulability. If someone in your family indeed had a problem with deep veins thrombosis, it doesn’t necessarily mean that you will develop it, because genetic predisposition usually has to be combined with other risk factors.
Pregnancy
Women who are pregnant or have recently given birth are in increased risk. Pregnant women produce more blood for fetuses needs, more pressure is done on a pelvis and legs, and their body mass is increased.
Cancer
Some types of cancer, especially lung, pancreatic, ovarian, or breast cancer are increasing the chance for blood clot forming.
Oral contraceptives
Women who use high estrogen oral contraceptives or hormonal replacement therapy have an increased risk for deep vein thrombosis.
Obesity
The excess of body fat is causing an estrogen increase. Because the estrogen stored in adipose tissue may increase the risk for blood clotting or other inflammations. The additional weight is making higher pressure on veins of pelvis and legs.
Age
People older than the age of 60 have an increased risk for deep vein thrombosis development, and those older the 75 are at the highest risk, especially if they have other risk factors.
Smoking
Smoking is a risk factor for blood clotting in itself, but it is also amplifying other risk factors.
Complications
The most serious complication of deep vein thrombosis is a pulmonary embolism.
Pulmonary embolism
Pulmonary embolism occurs when the thrombus is torn from its original location, moving through the circulation, and stopping in the arteries in the lungs. Because the blood flow is stopped, it can lead to permanent damage, or even cause sudden death. If the symptoms of pulmonary embolism are showed, immediate seeking of medical help is needed.
Pulmonary embolism symptoms
- Shortness of breath. Wheezing and other troubles with breathing may occur.
- Chest pain/discomfort. This manifestation may look like heart attack symptoms.
- Tachycardia. A faster heart rate.
- Tachypnea. Abnormal rapid breathing.
- Hemoptysis. A coughing up of blood or blood-stained mucus.
- Syncope. Fainting, a loss of consciousness and muscle strength.
- Pulmonary embolism is a life-threatening condition, and the first sign of it may be the sudden death. So many of pulmonary embolism cases are diagnosed at the autopsy.
Postphlebitic syndrome
Deep vein thrombosis can lead to a postphlebitic (postthrombotic) syndrome. Symptomatic venous insufficiency develops after the damage from blood clots, reducing the blood flow. The symptoms of this disorder are:
- Persistent leg swelling.
- Leg pain, cramps, and tingling which amplify when walking or standing, and weaken while laying down with an elevated leg.
- Skin discoloration.
- Varicose veins. Veins are enlarged and twisted.
- Venous ulcer. The wounds on veins which can be painful, lowering the quality of life.
- Dermatitis. Also known as eczema, a skin inflammation is caused by stasis in veins.
Diagnosis
Medical history and physical examination help in the diagnosis of deep vein thrombosis before further examinations. Diagnose is confirmed with blood tests, ultrasound, venography, or MRI.
Blood tests
The concentration of the substance called D-dimer is elevated in deep vein thrombosis. D-dimer is the degradation product of fibrin. This test is very sensitive, but not so specific, meaning that the elevated concentration does not certainly mean that there is deep vein thrombosis. However, the negative results help in excluding this condition.
Ultrasound
Ultrasound can identify a blood clot directly by sending sound waves which can produce a picture of venous endothelium. This test is more specific for upper leg veins than for veins of a lower leg. Ultrasound is not an invasive procedure, it is safe and painless, as it does not emit any harmful waves.
Venography
Venography is invasive, but the most specific test for diagnosing the deep vein thrombosis, although it isn’t performed very often due to its cost and invasiveness. It is based on X-ray imaging of the veins where the contrast dye is inserted via catheter continually. Blood clots and other vein problems may be found with this test.
MRI
Magnetic resonance imaging can provide a visual image using radio waves and a strong magnetic field, which can show if there is a clot or some other problem in the vein.
Treatment
The goals for deep vein thrombosis treatment are:
- Primary prevention
- Treating the blood clot in the acute phase
- Secondary prevention
Primary prevention
Primary prevention is the prevention of deep vein thrombosis in people who haven’t developed this disease but are at high risk.
Non-pharmacological measures
Regular exercises are recommended, especially for people whose work is based on long traveling or sitting. Exercises lower the risk for blood clot forming. The best type of exercises, in this case, are aerobic exercises combined with anaerobic exercises. Stop smoking, as smoking is increasing the chance for blood clot forming, particularly if it’s combined with other risk factors. Compression stockings help in relieving of the pressure, pain, and swelling in the leg. These garments are contraindicated in people with poor arterial circulation like the people with severe heart failure. If you are on a long journey, do get up and walk a little bit from time to time. If you had surgery recently, try to get up and walk as soon as you can. When you are laying in the bed, put some pillows below your legs to keep them elevated.
Pharmacological measures
Pharmacological measures in prevention include the use of parenteral and oral anticoagulants (blood thinners). They are usually indicated in leg orthopedic surgeries.
Deep vein thrombosis treatment
The goal in deep vein thrombosis treatment is to break down the blood clot or to stop its expansion, reducing the risks of chronic complications, and to prevent the recurrent deep vein thrombosis. Pharmacological treatment usually begins with a parenteral anticoagulant. Within the first 24 – 48h the warfarin is given. The inadequate anticoagulation therapy in the first 24 hours may increase the risk of pulmonary embolism. Alternatively, treatment can begin and be continued with new anticoagulant drugs. In the most severe cases with a very high risk of embolization, the use of thrombolytics (clot busters) is required.
Parenteral anticoagulants
Parenteral anticoagulants include heparin, low molecular weight heparins (LMWH), and synthetic pentasaccharide inhibitors of factor Xa such as fondaparinux.
Heparin’s mechanism of action is the activation of antithrombin III, which is blocking thrombin’s function in blood clotting. Heparin is a short-acting drug so it must be given frequently via injections (intravenously or under the skin), or via continuous infusion. Monitoring of heparin is required to ensure its anticoagulant activity. This is done by checking activated partial thromboplastin time (aPTT), which characterizes blood coagulation. Activated partial thromboplastin time needs to be 1.5 – 2.5 times normal values.
Low molecular weight heparins represent the heparin’s fragments. They are given via injections under the skin, lasting longer than regular heparin. LMWH can be given at home, unlike the heparin. They do not require monitoring, as they have fewer interactions and side effects.
Fondaparinux is a synthetic sugar composed of five sugars in heparin that are responsible for binding to antithrombin. It doesn’t need monitoring, and it has less side effects than heparin.
Oral anticoagulants
Oral anticoagulants include coumarins (vitamin K inhibitors) and new oral anticoagulants.
Warfarin is the dominant member of coumarins. its mechanism of action is the blocking of vitamin K’s activity in the carboxylation of clotting factors. It needs 2-3 days to fully manifest its effects. Many factors affect warfarin’s anticoagulant effect so it needs to be monitored. International Normalised Ratio (INR) represents the blood clotting tendency and its values should be above the 2.5 in deep vein thrombosis and above 3.5 for recurrent deep vein thrombosis or in patients with heart valve problems. Acenocoumarol is similar to warfarin, but it’s used less often.
New oral anticoagulant drugs include dabigatran which is a direct thrombin inhibitor, and rivaroxaban, apixaban, and edoxaban which are direct inhibitors of clotting factor Xa. Their effect starts after 2 – 3 hours, and they don’t need monitoring. New oral anticoagulants have fewer interactions, but they are expensive.
Thrombolytics (clot busters)
These drugs dissolve blood clots, converting plasminogen into plasmin. They are given in severe cases of deep vein thrombosis intravenously or via catheterization, directly into the affected area.
