Angiotensin II receptor blockers (ARBs)
Angiotensin II receptor blockers (ARBs), also known as “sartans” are the newer type of antihypertensives which act on the renin-angiotensin system. They are often prescribed if angiotensin-converting enzyme inhibitors cause side effects. First orally used, non-peptide, selective angiotensin II receptor inhibitor, losartan, was approved for clinical use in the United States in 1995, as the previous peptide analogs of angiotensin II like saralasin lacked the bioavailability. Many different angiotensin II receptor blockers were developed since then.
Angiotensin II
Angiotensin II is a potent vasoconstrictor which is involved in the regulation of blood pressure in the human body. Angiotensin-converting enzyme (ACE) transforms the angiotensin I, which doesn’t have any known physiological effects into angiotensin II. Drugs known as ACE inhibitors act on this stage, inhibiting the synthesis of angiotensin II, but this conversion isn’t completely blocked, as other enzymes such as chymase can perform this function. Besides the inhibition of angiotensin I transforming, ACE stops the degradation of bradykinin, which can cause some side effects, but also an improved decrease in blood pressure. Angiotensin II causes the narrowing of blood vessels (vasoconstriction) directly and by activating the sympathetic nervous system. Moreover, it induces the release of aldosterone, a mineralocorticoid hormone which elevates the blood pressure, favoring the retention of sodium and water, and increasing the volume of circulating blood.
Angiotensin II is associated with cardiac remodeling, changing its morphology and structure, thus worsening its function. It can induce migration, proliferation, and hypertrophy of the heart muscle cells, as well as the extracellular matrix forming.
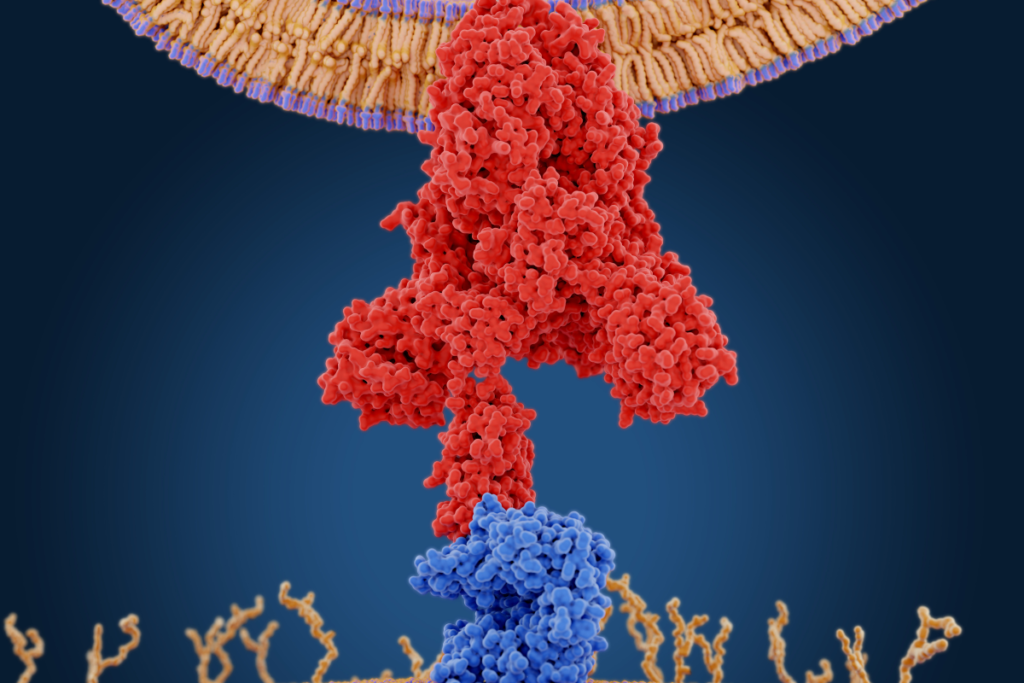
Angiotensin receptors
Angiotensin II performs its effects through at least two types of receptors, called AT1 and AT2. AT1 receptors are mainly located in the heart, brain, adrenal glands, liver, and kidneys. Through them. angiotensin II regulates the blood pressure, and sodium homeostasis, while AT2 receptors are mainly found in cells of the fetus, existing only in low levels in adults. Activation of AT1 receptors induces blood vessel narrowing, a release of aldosterone, secretion of vasopressin (antidiuretic hormone), cardiac remodeling, activation of the sympathetic nervous system, and other effects.
Examples
Angiotensin II receptor blockers are divided by their affinity for AT1 receptors, referring to how specifically are the drugs bound to AT1 receptors; by their biological half-life, a time which is needed to pass for half of the drug to be removed from the organism; or by their elimination and distribution in the body. Some of the ARBs are prodrugs, so they achieve their active form, after the metabolic conversion in the human body. They are usually administered once per day. Examples of angiotensin II blockers are losartan, valsartan, telmisartan, irbesartan, azilsartan, candesartan, olmesartan, eprosartan, and fimasartan.
Mechanism of action
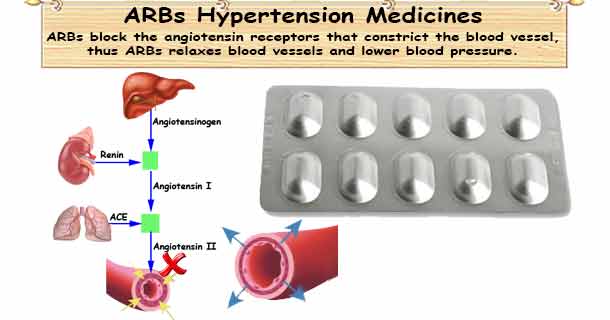
Angiotensin II receptor blockers are competitive antagonists of AT1 angiotensin II receptors, and that inhibition is insurmountable, meaning that the angiotensin II can’t manifest its full effects even if it’s in elevated concentration. The angiotensin II cannot overcome the inhibition of AT1 receptors, but this inhibition is reversible. They don’t affect the degradation of bradykinin, a vasodilator which is responsible for side effects like dry cough and angioedema in ACE inhibitors use.
Indications
Angiotensin II receptor blockers are used in several heart-related disorders, although its main indication is hypertension, as they primarily reduce high blood pressure. The other conditions where ARBs are used are heart failure, diabetic nephropathy, and other chronic kidney diseases. They can also be used in long-term therapy of heart attack.
Hypertension

Hypertension or high blood pressure is a condition where blood pressure surpasses the value of 140 / 90 mm Hg. Angiotensin II receptor blockers are commonly prescribed if ACE inhibitors cause side effects, but recently they’re prescribed more and more besides the people who don’t tolerate ACE inhibitors. They block the effects of angiotensin II, lowering the peripheral resistance and blood pressure. Similarly to ACE inhibitors their mechanism of action involves renin-angiotensin system, but at a different stage. This is the reason why ARBs have fewer side effects and are generally well tolerated. They don’t cause dry cough as they don’t affect the degradation of bradykinin.
Heart failure
Heart failure is a heart disease where the heart can’t adequately supply the organs and peripheral tissues with oxygen and nutrient-rich blood. ARBs are usually prescribed in heart failure if a patient can’t tolerate ACE inhibitors because of persistent dry cough or angioedema. By selectively blocking the AT1 receptors, ARBs decrease the vasoconstriction, bad blood flow through the vital organs, retention of water and sodium, as well as cardiac remodeling. They reduce the preload (the amount of ventricular stretch during the diastole), reducing the heart failure symptoms like leg and ankle swelling and pulmonary edema, and the afterload (the resistance that the heart needs to overcome to pump the blood into circulation), thus improving the pumping ability of the heart and its stroke volume.
Heart attack

A heart attack is a condition that occurs if one or more of the blood vessels which supply the heart get obstructed, causing the heart muscle cells to die. Angiotensin II receptor blockers are given in long-term therapy of the heart attack if ACE inhibitors can’t be used. The main goal for this therapy is the prevention of cardiac remodeling, as it can occur after the heart attack, causing it to change its shape, structure, and size, worsening its function. ARBs inhibit the initiation of angiotensin II effects on AT1 receptors on the heart’s cells, preventing cardiac remodeling. They also benefit the heart as they reduce the preload, afterload, and the activity of the sympathetic nervous system.
Diabetic nephropathy
Diabetic nephropathy represents one of the complications of diabetes that affects the kidneys, as the high concentration of blood sugar, glucose damages the structure of kidneys responsible for glomerular filtration. Injuries developed on the kidney may cause a leakage of proteins into the urine, a condition known as proteinuria. As the disease progress, it may lead to a life-threatening condition, kidney failure, an end-stage kidney disease, but this situation rarely occurs. Angiotensin II receptor blockers decrease the high blood pressure which can additionally damage the kidneys, they reduce the proteinuria with their renoprotective effects, and therefore conserve the kidney function.
Chronic kidney disease
Chronic kidney disease is a disorder where kidneys lose their function over time, letting the toxic waste and water to accumulate in the organism. ARBs manage hypertension due to their vasodilating effects, promoting the perfusion of the kidney, and improving the renal ischemia and hypoxia. They also reduce the proteinuria, protecting the kidney cells.
Contraindications
Angiotensin II receptor blockers shouldn’t be used in certain conditions, as they can worsen them. Such appearances include pregnancy, bilateral renal artery stenosis, or unilateral renal artery stenosis in sole functioning kidney, hypotension, and hyperkalemia.
Pregnancy
Angiotensin II receptors blockers are contraindicated in pregnancy and breastfeeding, as angiotensin II is an important element in fetal development. They are teratogenic drugs, meaning that they can induce developmental malformation, including renal function impairment, oligohydramnios (a deficiency of amniotic fluid), calvarial hypoplasia (a deficiency in skull forming), and even death of the fetus. As pregnant women shouldn’t use ARBs, they need to treat hypertension with other methods.
Renal stenosis
If a patient with bilateral renal artery stenosis or unilateral stenosis of the sole functioning kidney use angiotensin II receptors, they may develop kidney failure as angiotensin II is maintaining the balance between the afferent arteriole (a blood vessel that is leading the blood into kidney), and efferent arteriole (a blood vessel that leads the blood from a kidney), by narrowing the efferent arteriole. So if ARBs are used, they remove the constricting effect on efferent arteriole, disrupting the difference in pressure, and glomerular filtration rate because the afferent arteriole in stenosis is already narrowed, and it needs to be more dilated than efferent arteriole for filtration to happen.
Hypotension
A state of hypotension represents the blood pressure below the 90 / 60 mm Hg. As angiotensin II receptor blockers decrease the blood pressure, an extremely lowered blood pressure may induce a shock, which can be a life-threatening event.
Hyperkalemia
Hyperkalemia represents the elevated concentration of potassium ions (K+) in blood. This is a dangerous condition, manifested through muscle pain, muscle weakness or numbness, and palpitations. It can invoke serious heart rhythm abnormalities which can lead to cardiac arrest. ARBs shouldn’t be used in this condition, as they increase the potassium levels in the blood.
Side effects
Angiotensin II receptor blockers are relatively well-tolerated medications, but like all other drugs, they can cause some side effects.
- hypotension – ARBs can reduce the blood pressure below normal levels like all other antihypertensive medications, mostly if they are combined with other drugs from this class
- dizziness, headache, tiredness – effects that may happen due to vasodilating effects
- hyperkalemia – elevated concentration of potassium ions (K+) may occur due to decreased secretion of aldosterone whose main function is to preserve sodium and water, and to eliminate the potassium
- acute renal failure – a serious, life-threatening condition that may occur if ARBs are used in bilateral artery stenosis, or unilateral stenosis of the sole functioning kidney
- altered taste sensitivity – angiotensin II receptor blockers may cause a sensation of metallic or salty taste
- sexual dysfunction – a problem that may be associated with all antihypertensive types
- angioedema – a dangerous tissue swelling that can rarely occur in ACE inhibitors use, and it’s even less commonly in angiotensin II receptor blockers usage
- digestive system problems – a possible side effects of almost any drug
Interactions
Angiotensin II receptor blockers can interact with other medications, so it’s important to tell which medications are you taking to your doctor or your pharmacist.
NSAID
Nonsteroidal anti-inflammatory drugs can interact with ARBs on several levels. NSAIDs can lower the antihypertensive effects of ARBs, increase potassium levels, and induce kidney failure in patients with hypoperfusion of kidneys. These combinations should be monitored, particularly in elderly people. It is sometimes needed to monitor the kidney function also.
Potassium-sparing diuretics
Potassium-sparing diuretics are commonly prescribed with other antihypertensives, but since both potassium-sparing diuretics and ARBs lead to an increase in potassium ion (K+) levels in the blood, their combination should be avoided.
Lithium
Lithium is a drug that is mainly used for bipolar disorder treatment. If it’s used during the therapy with angiotensin II receptor blockers, its concentration in the blood may rise and lead to an expression of its toxic effects.
