Thrombolytics
Thrombolytics, also known as fibrinolytics or clot-busting agents are the type of drugs used to treat various conditions related to blood vessel occlusion done by a thrombus. This type of therapy begun in the middle of the 20th century, but the modern way of thrombolytic agent use started in the 90’. In 1933, an American scientist William Tillet has found that beta-hemolytic streptococci are capable of synthesizing a thrombolytic substance, which was later named streptokinase. At first, streptokinase was used to treat other diseases such as empyema, hemothorax, and tuberculous meningitis, while a couple of decades later, in 1958 they started to use it in patients with a heart attack. After the streptokinase, scientists have found and designed several other thrombolytic drugs, and this therapy has shown to improve the survival rate of thrombus-related conditions.
Fibrinolysis

Hemostasis is a process which is responsible for stopping of the bleeding, and it is divided into four stages including vasoconstriction (blood vessel narrowing), plug forming, coagulation (blood clotting), and in the end the stabilization and breakdown of blood clots by fibrinolysis. Blood clots are an important factor of blood vessel injury heal, but if they form inside the blood vessels, without the bleeding, that pathological process is called thrombosis.
Fibrinolytic system is enabling the injury heal and the breakdown of a blood clot. After the coagulation, the fibrinolytic system takes the role of clot elimination, with the process of enzymatic clot elimination, called fibrinolysis. Plasmin is an enzyme that breaks down the fibrin, and it forms after the changing of its inactive form plasminogen, which is synthesized in the liver. Plasminogen is physiologically activated by tissue plasminogen activator (tPA) and urokinase (uPA). Tissue plasminogen activator is produced by endothelial cells, and during the coagulation, it binds to fibrin, which increases the speed of its fibrinolytic ability for plasminogen activation. Urokinase, also known as urokinase-type plasminogen activator is another enzyme responsible for the conversion of plasminogen. It was originally isolated from the human urine, so it was named after that.
Types
The most commonly used thrombolytic agents include alteplase, which represents the recombinant form of human tissue plasminogen activator, reteplase and tenecteplase, derivatives of recombinant tissue plasminogen activator, streptokinase, a protein purified after it’s produced by streptococci bacteria, anistreplase, a complex of purified human plasminogen and acylated streptokinase, and urokinase, an urinary-type plasminogen activator, synthesized in kidneys.
Mechanism of action
The mechanism of action of the thrombolytic drugs relies on the conversion of the plasminogen into its active form – plasmin. Tissue plasminogen activators bind to fibrin on the clot’s surface activating the plasminogen, converting it to the plasmin. Plasmin is a proteolytic enzyme that then breaks the fibrin molecules, dissolving a blood clot. Streptokinase is a protein from streptococci with a different structure than tissue plasminogen activators. It activates plasminogen directly by forming complexes with plasminogen, releasing the plasmin in the circulation.
Indications
Thrombolytics are used in a number of conditions related to thrombotic occlusions of blood vessels including heart attack, stroke, deep vein thrombosis, pulmonary embolism, and acute peripheral arterial occlusion.
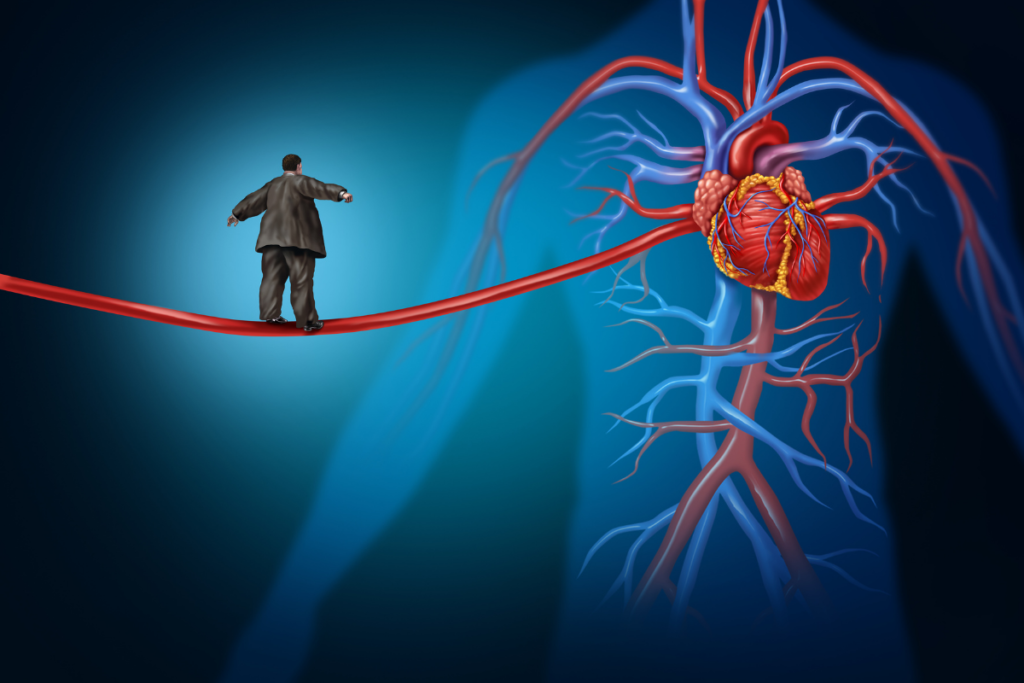
Heart attack

A heart attack occurs when the oxygen and nutrient-rich blood supply is cut off from the part of the heart, resulting in heart muscle cell death. ST-segment elevated myocardial infarction (STEMI) occurs when some of the arteries that supply the heart get completely obstructed, where the elevated ST stands for a change on ECG. This is a life-threatening emergency that must be treated quickly. Thrombolytics are given to dissolve a blood clot that blocked the coronary blood flow. They must be given within the 24 hours since the heart attack (often within the 12 hours, because the sooner they are given, the greater is the chance for survival and heart muscle preservation. These drugs are applied intravenously, and they are most often used when PCI (percutaneous coronary intervention) couldn’t be done.
Stroke
A cerebrovascular insult, also known as a stroke occurs when a brain cells die due to the inadequate blood supply. Stroke can be ischemic or hemorrhagic. Thrombolytics are used in the treatment of ischemic stroke if it’s induced by an embolus, a torn atherosclerotic plaque, as opposed to hemorrhagic stroke where they’re contraindicated. Alteplase needs to be applied as soon as possible to increase the chance of survival and lower the complications, intravenously within the 4.5 hours since the stroke occurrence, or within the 6 hours if it’s given via endovascular tube directly into the affected blood vessel.
Deep vein thrombosis

A heart attack occurs when the oxygen and nutrient-rich blood supply is cut off from the part of the heart, resulting in heart muscle cell death. ST-segment elevated myocardial infarction (STEMI) occurs when some of the arteries that supply the heart get completely obstructed, where the elevated ST stands for a change on ECG. This is a life-threatening emergency that must be treated quickly. Thrombolytics are given to dissolve a blood clot that blocked the coronary blood flow. They must be given within the 24 hours since the heart attack (often within the 12 hours, because the sooner they are given, the greater is the chance for survival and heart muscle preservation. These drugs are applied intravenously, and they are most often used when PCI (percutaneous coronary intervention) couldn’t be done.
Pulmonary embolism
Pulmonary embolism is a condition caused by an obstruction of the artery in the lungs. In most cases it resembles a complication of deep vein thrombosis when a thrombus formed in deep veins in legs (commonly upper leg) gets torn from its original location and travels through the circulation, stopping in an artery inside the lung. In severe cases, where the thrombus doesn’t dissolve on its own, an usage of thrombolytics is needed.
Acute peripheral arterial occlusion
If a peripheral artery gets acutely obstructed by a torn thrombus, causing pain, coldness, tingling sensation, thrombolytic drugs may be used to breakdown the thrombus which caused it.
Contraindications
Like all other drugs, thrombolytic agents shouldn’t be used in certain conditions, as it could lead to dangerous consequences. They are generally safe, but the bleeding may represent a serious problem. Contraindications may be divided into absolute and relative contraindications.
Absolute contraindications
Some of the important states and conditions where thrombolytic agents should be absolutely avoided include
- prior intracranial hemorrhage (hemorrhagic stroke)
- ischemic stroke, within 3 months
- recent cranial surgery or injury
- intracranial neoplasm (brain tumor)
- suspected aortic dissection
- severe, uncontrolled hypertension (unresponsive to emergency therapy)
- active bleeding (excluding the normal bleeding during menstruation), or bleeding disorder
Relative contraindications
Some of the important states and conditions where thrombolytic agents should be avoided if it’s possible include
- remote ischemic strokes > 3 months
- major surgery, within 3 months
- recent internal bleeding within 2 to 4 weeks
- after the 75 years of age
- active peptic ulcer
- pregnancy
- current use of anticoagulant drugs
- dementia
- bacterial endocarditis or pericarditis
- liver dysfunction such as liver failure, cirrhosis, and active hepatitis
- acute pancreatitis
Side effects
Like other drug classes, thrombolytics have a few side effects that may be expressed in certain people. Some of them include:
bleeding – as thrombolytic dissolve the thrombus, they can cause bleeding which can sometimes be severe and dangerous; they can induce bleeding gums, easy bruising, nosebleeds, internal bleeding, a bleeding inside the stomach or intestines (expressed via blood in feces – dark stool), bleeding inside the kidneys (blood in urine), bleeding inside the muscles (muscle pain), heavy menstrual bleeding, and rarely but with possible serious consequences bleeding inside the brain*; they can also cause bleeding from surgical incisions and needle shots
intracranial bleeding* – a rare but, dangerous side effect manifested through the dizziness, convulsions, hemiparesis (weakness of the one entire side of the body), or slurred speech; hemorrhagic stroke, is a potentially fatal but very rare side effect
- fever
- low blood pressure
Interactions of thrombolytics with other drugs
Thrombolytics may come in interactions with other drugs, so it’s important to tell your doctor or your pharmacist which drugs you are taking. Some of the important interactions include the ones with:
Anticoagulants (Blood Thinners)
Anticoagulants are the drugs that are used to prevent the blood clotting and to reduce the chance of life-threatening events related to clotting. Since they affect the clot forming and increase the risk of bleeding, their use with thrombolytics which can also increase the bleeding occurrence, additionally enhance these effects.
Antiplatelet drugs
Antiplatelet drugs are used to prevent arterial thrombosis in various cardiovascular conditions. All drugs of this class may induce bleeding due to their mechanism of action in preventing the platelet plug forming. Simultaneous use of antiplatelet drugs and thrombolytic agents may furthermore increase the chance of bleeding.
NSAIDs
The use of nonsteroidal anti-inflammatory drugs and thrombolytics increases the chance of gastric ulcer occurrence or the gastric bleeding occurrence.
Antihypertensives
Antihypertensive drugs used to treat high blood pressure can lead to hypotension (abnormally low blood pressure) in some cases, and this effect may be enhanced by thrombolytics.
