Antiplatelet drugs

Antiplatelet drugs are widely used to prevent arterial thrombosis in various cardiovascular-related conditions. Acetylsalicylic acid (aspirin), is a famous drug used since ancient times, and even then it was known that plants which contain salicylate such as willow can reduce the pain and fever. In 1897, a German scientist Felix Hoffman who was working for Bayer has synthesized aspirin. Later, in the mid 20th century, aspirin’s true mechanism of action was found and clinical tests have shown that it decreases the risk of diseases related to thrombosis. A number of antiplatelet drugs have been developed and synthesized since then.
Platelet plug forming (platelet aggregation)
Platelet plug aggregation is a part of hemostasis, a process responsible for stopping of bleeding. Hemostasis is divided into four stages, starting with blood vessel narrowing (vasoconstriction), going through platelet plug formation, then blood clotting (coagulation), and finally finishing with stabilization and breakdown of blood clots with a process called fibrinolysis.
A platelet plug is necessary for stopping of bleeding and recovery of vascular injuries, but if it occurs in unwanted location, it leads to thrombosis, a pathological obstruction of blood vessels. It is consisted of thousands of platelets, mechanically patching the injured blood vessel. A platelet plug stops the bleeding temporarily, but it also represents the base for a blood clot. If a blood vessel suffers some minor damage, or a small blood vessel is injured, that plug can stop the bleeding completely.
The normal uninjured endothelial wall of a blood vessel is smooth, reflecting the platelets and coagulation factors. When it gets injured, that reflection stops, platelets adhere to the endothelial wall and get activated, changing their shape, emptying the granules stimulating further interaction between them causing aggregation. ADP (Adenosine diphosphate) is causing the adhesion of new platelets, stimulating additional degranulation and aggregation, while thromboxane A2 activates new platelets who express Iib/IIa receptors, while it also causes vasoconstriction (blood vessel narrowing). Massive platelet aggregation is resulting in platelet plug forming.
Types and mechanisms of action of antiplatelet drugs
Many types of antiplatelet drugs exist, but the 3 main types are irreversible cyclooxygenase (COX) inhibitors, adenosine diphosphate (ADP) receptor inhibitors, and glycoprotein IIb/IIa inhibitors.
Irreversible cyclooxygenase inhibitors
The representative of this group is acetylsalicylic acid (aspirin). Aspirin is the most commonly used antiplatelet agent. Its mechanism of action relies on irreversible inhibition of an enzyme called cyclooxygenase. Platelets don’t have a nucleus so they can’t replenish their cyclooxygenase, meaning that that inhibition lasts for a whole lifespan of a platelet (up to 10 days). Cyclooxygenase is responsible for the synthesis of thromboxane A2 which causes vasoconstriction, and its interrupted synthesis inhibits the platelet aggregation.
Adenosine diphosphate (ADP) receptor inhibitors
This group of antiplatelet agents inhibits the P2Y12 receptors which represent the receptors for platelet activating factor ADP, thus they prevent the platelet aggregation. Examples of ADP diphosphate receptor inhibitors include clopidogrel, prasugrel, ticagrelor, ticlopidine, and others.
Glycoprotein IIb/IIa inhibitors
Glycoprotein IIb/IIa inhibitors bind directly to glycoprotein IIb/IIa receptors on the surface of the platelets inhibiting them. Those receptors are responsible for platelet aggregation and binding of fibrinogen. Fibrinogen is a soluble protein that is converted into insoluble protein fibrin which makes the thrombus. Examples of glycoprotein IIb/IIa inhibitors are abciximab, eptifibatide, and tirofiban.
Indications of antiplatelet drugs
Antiplatelet drugs are used to prevent the forming or an expansion of the thrombus in the arterial circulation, where anticoagulants show little effect. They are used in the prevention and treatment of acute coronary syndrome (including heart attack and unstable angina), stroke or TIA, stable angina, peripheral artery disease, and in percutaneous coronary intervention.
Acute coronary syndrome
When the blood vessel that supplies the heart gets obstructed completely, heart muscle cells die due to an inadequate supply of oxygen and nutrient-rich blood, and that condition is called a heart attack (myocardial infarction). When the blood vessel is not obstructed completely, or for a short time, that condition is called unstable angina. Both those conditions are part of an acute coronary syndrome. When the heart attack occurs, a tablet of aspirin in higher concentration needs to be chewed to act rapidly, and other antiplatelet medications might be given. Life-long therapy of aspirin in a concentration of 75 or 100 mg is needed after the survived heart attack or after unstable angina attack. Clopidogrel may be used if aspirin is contraindicated. Clopidogrel, prasugrel or ticagrelor are used along with aspirin for 12 months after percutaneous coronary intervention. Glycoprotein IIb/IIa antagonists are used if the risk for heart attack is high after an unstable angina attack.
Stable angina

Angina pectoris is a pain or pressure felt in the chest, and it is the main symptom of ischemic heart disease caused by atherosclerosis. Stable angina represents a predictable chest pain. Aspirin reduces the ability of platelet aggregation, easing the blood flow throughout the atherosclerotic, narrowed arteries, also reducing the risk for heart attack. Other antiplatelet drugs can be used if aspirin is contraindicated.
Stroke and TIA
Stroke or a cerebrovascular infarction is a condition where brain cells die due to an inadequate blood supply. Arterial obstruction causes an ischemic stroke, blood flow is stopped and cells in ischemic zone die. TIA (transient ischemic attack) occurs when the blood supply in the brain is stopped temporarily, but it recovers completely afterward. Antiplatelet therapy is used in ischemic stroke and TIA treatment, as opposed to hemorrhagic stroke (caused by a rupture of blood vessel in the brain), where they can worsen the condition. Aspirin may be used in the prevention of stroke if a patient has a high risk for cardiovascular diseases. After a stroke or TIA occurrence, aspirin is used in combination with clopidogrel, both in low doses. Long-term prevention of stroke reappearing includes the use of aspirin, clopidogrel or aspirin + dipyridamole dual therapy.
Peripheral artery disease
Peripheral artery disease represents the narrowing of peripheral arteries. Limbs have lowered blood flow and symptoms express commonly in legs, causing pain while walking (claudication). Aspirin or clopidogrel are used to prevent platelet aggregation and to ease the blood flow through the narrowed arteries.
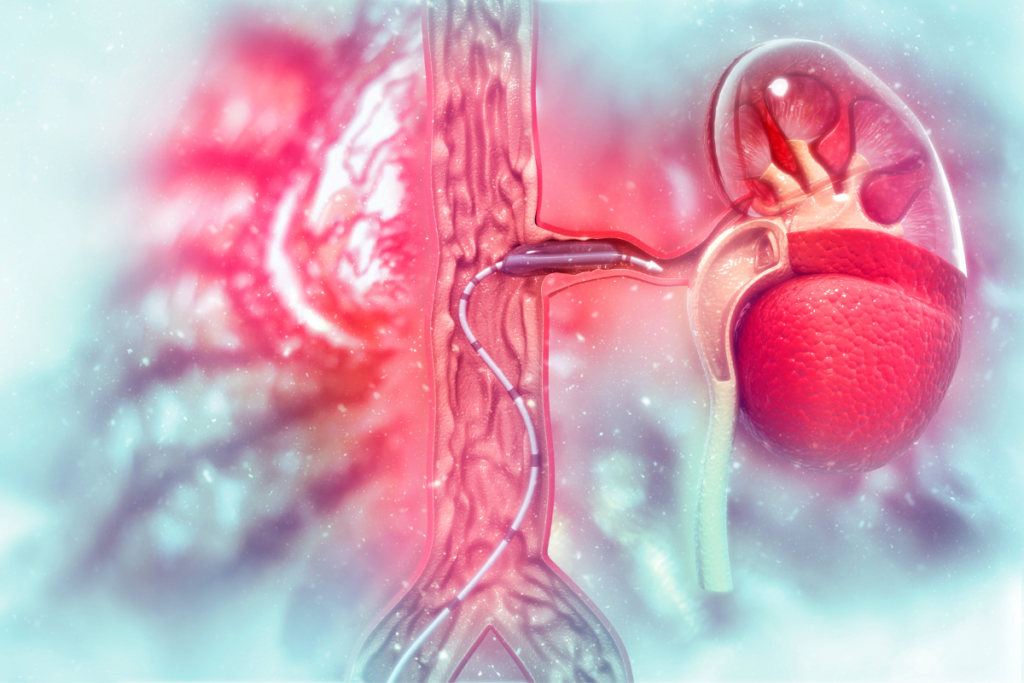
Percutaneous coronary intervention
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of coronary arteries. A long tube is entered through the femoral or radial artery and navigated to the narrowed site. Tip of the tube may have a balloon shape and when it’s inflated it widens the problematic artery. After the balloon angioplasty, a stent may be inserted to keep the artery open. After placement of a stent, aspirin and clopidogrel combination in low doses is recommended for 12 months.
Contraindications
Antiplatelet drugs shouldn’t be used in certain conditions as they could cause some health complications. Those states and conditions include active bleeding, children under the age of 16, last trimester of pregnancy, asthma, and severe kidney or liver dysfunction.
Children under the age of 16
Children under the age of 16 should avoid using aspirin, especially if they have chickenpox or flu-like symptoms as it could cause a Reye’s syndrome. It is a rare, but serious condition that is characterized by swelling in the brain and liver. Reye’s syndrome is a life-threatening condition that requires immediate care. It is manifested through confusion, vomiting, seizures, and loss of consciousness.
Pregnancy
Aspirin shouldn’t be used in the last trimester of pregnancy because it inhibits the synthesis of prostaglandins which are important factors for organ development in fetuses. A cavity between the left and right side of the heart could get sealed prematurely, and fetus can develop pulmonary hypertension. Also, renal dysfunction can occur, leading to kidney failure. Prostaglandins are important for contractions of the uterus, and their deficit can prolong the time of labor and bleeding. Besides that, other antiplatelet drugs should be avoided in pregnancy as there are not enough data about their effects on fetal development.
Asthma
Aspirin should be avoided or used with caution in people with asthma as it could increase the bronchoconstriction (narrowing of airways). Because the aspirin blocks the COX, leukotrienes are formed by lipoxygenase’s effect on arachidonic acid. Leukotrienes cause the bronchial muscles to contract, inducing the wheezing and difficulty in breathing.
Side effects
Like all other medications, antiplatelet drugs can cause some side effects.
- bleeding – all antiplatelet drugs may cause bleeding, as they prevent platelet plug forming which decrease hemostasis; some antiplatelet drugs have a higher chance to induce the bleeding than others, meaning that ADP receptor inhibitors have lower risk to induce hemorrhage than aspirin; it is mainly manifested with nosebleeds, bleeding gums, gastrointestinal bleeding, prolonged bleeding from an injury or prolonged menstrual bleeding, while in some people a heavy bleeding associated with blood in feces, urine or vomit may occur.
- gastrointestinal problems – digestive system problems including dyspepsia, gastric ulceration, and hemorrhage, or perfusion of a gastric ulcer are also more commonly expressed in aspirin use than in use of ADP receptor inhibitors;
- Reye’s syndrome and worsening of asthma – side effects of aspirin
- thrombocytopenia – a number of thrombocytes (platelets) below normal values; it could be induced by glycoprotein IIb/IIa inhibitors or ticlopidine
- neutropenia – neutropenia represents an abnormally low number of neutrophils, a type of leukocytes (white blood cells), which makes the affected person more vulnerable to infections; ticlopidine may cause neutropenia
Interactions
Antiplatelet drugs may come in interaction with other medications including the other antiplatelet drugs, anticoagulants, and thrombolytics (fibrinolytics, clot busters), which increases the risk of bleeding, so it’s important to tell your doctor or a pharmacist which medications are you using. Some drugs that come in important interaction with antiplatelet drugs are:
Methotrexate
Methotrexate is a drug used in the treatment of autoimmune disorders such as rheumatoid arthritis, psoriasis, and Crohn’s disease, as well as in cancer treatment. If it’s used along with aspirin, its concentration in blood may rise, and cause toxic effects including fever, mouth sores, unusual bleeding or bruising.
Ibuprofen
Ibuprofen can reduce the antiplatelet activity of aspirin, and decrease its cardioprotective effects.
Uricosurics
Uricosurics are drugs that are used to treat gout, increasing the elimination of uric acid from the blood. Aspirin can decrease their effect as it increases the uric acid level in blood.
Digoxin
Digoxin is used to treat atrial fibrillation or heart failure. Aspirin can increase the digoxin levels in the blood leading to toxic effects.
NSAIDs
Combination of aspirin with some of the other nonsteroidal anti-inflammatory drugs (NSAIDs) may increase the risk of gastric ulcer of gastric bleeding.
Proton-pump inhibitors
Proton-pump inhibitors are drugs that reduce the stomach acid production used in various diseases, among others in the prevention of gastric problems related to NSAID use. Omeprazole, a proton-pump inhibitor may reduce the effects of clopidogrel, as it interferes with its metabolism.
