Cardiac glycosides (Digoxin)
Cardiac glycosides are a class of organic substances that have an effect on the heart, and their only commonly used representative is digoxin. People have known for these drugs since ancient times, and throughout history, they were using them to treat various conditions including congestive heart failure, but also as a poison applied on arrows. In 1775, an English scientist William Withering described the clinical effects of an extract of the foxglove (Digitalis). The significant accomplishment was the standardization of digitalis preparations for clinical testing, finding the right dosage and avoiding toxicity. With the advance of science, the true mechanism of action of the cardiac glycosides was later found and described.
Na+/K+-ATPase
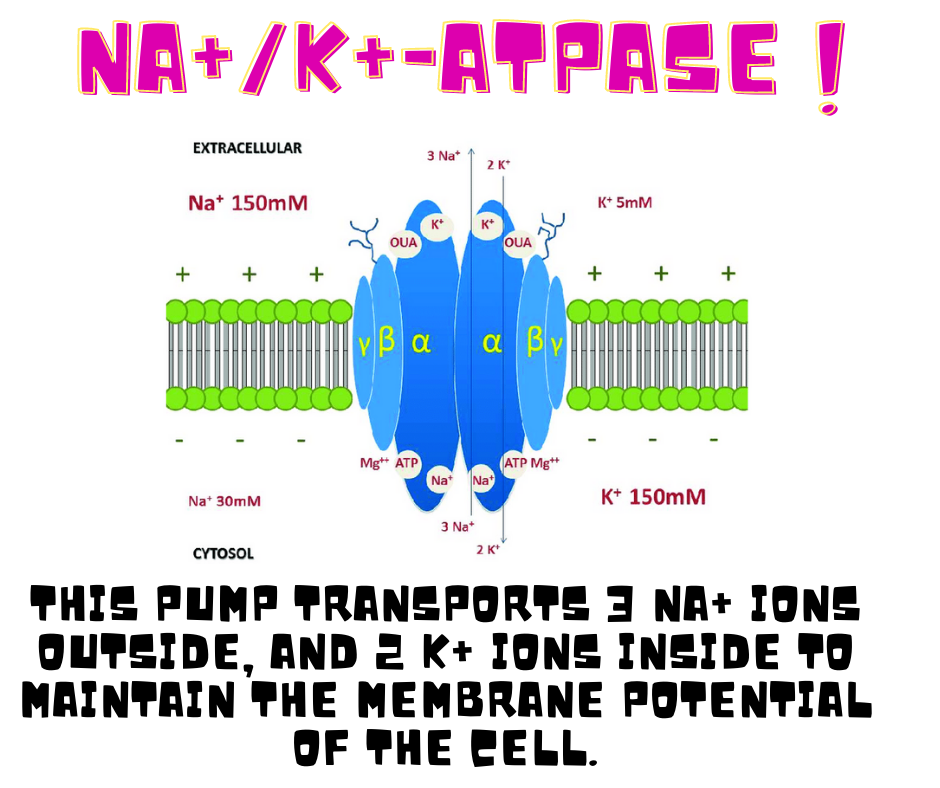
Na+/K+-ATPase is an enzyme located on the plasma membrane of the cell whose function is to pump the sodium ions out of the cell against its concentration gradient and to pump the potassium ions into the cell, also against its concentration gradient. This function is important for keeping the resting potential on the cell membrane because it keeps the large excess of K+ ions inside the cell and the high concentration of the Na+ ions outside the cell. Na+/K+-ATPase is an active transporter as it uses the energy acquired by hydrolysis of ATP (Adenosine triphosphate). This pump transports 3 Na+ ions outside, and 2 K+ ions inside to maintain the membrane potential of the cell. Furthermore, Na+K+-ATPase is important for the transportation of other ions, glucose, and amino acids.
Types
There are several cardiac glycosides including digitoxin, acetyldigitoxin, ouabain, deslanoside, but the most commonly used one is digoxin. It is a drug with a narrow therapeutic index, meaning that there is a small difference between the therapeutic and toxic concentration of the drug in the blood, so its use should be monitored, and the dose well adjusted. Digoxin is mostly applied orally in the form of tablets, but it could be used via intravenous infusion if it’s necessary.
Mechanism of action
Mechanism of action of digoxin relies on blocking of Na+K+-ATPase enzyme on heart cells’ membrane by binding to its extracellular α subunit, thus leading to an increased concentration of Na+ ions inside the cell. An increased concentration of Na+ ions is causing the increase of Ca2+ ion levels inside the cell because the function of the sodium-calcium exchanger (Na+/Ca2+ exchanger) function is decreased, as it normally transports 3 Na+ ions inside the cell and 1 Ca2+ ion outside to increase the concentration of sodium ions inside the cell if it’s low.
Calcium ions are also released from the sarcoplasmic reticulum, an organelle located inside the cell. Liberated Ca2+ is binding to a troponin C which removes the tropomyosin from actin and myosin filaments, leading to muscle contractions. Digoxin’s main effects are the increase in contractility of the heart muscle cells (positive inotropic effect), a decrease of heart rate (negative chronotropic effect), via depression of Sinoatrial node, a natural pacemaker of the heart, and the reduction in electrical conduction velocity (negative dromotropic effect), through the depression of the AV node.
Indications of Digoxin
Digoxin is used in the treatment of a couple of cardiovascular diseases including heart failure, atrial fibrillation, and supraventricular arrhythmias.
Heart failure
Heart failure is a condition where the heart’s function is decreased so it can’t adequately supply the organs and peripheral tissues with oxygen and nutrient-rich blood. Digoxin isn’t the first choice for treatment of heart failure, but it’s used if other drugs haven’t shown significant effects, and if the heart failure is accompanied by atrial fibrillation. It regulates the symptoms of heart failure, maintaining the patient’s ability to walk and exercise, improving the heart’s function, while reducing the number of hospitalizations, but it does not lower the mortality. It is indicated in heart failure with impaired systolic function, Digoxin improves heart contractility (positive inotropic effect), without affecting the heart muscle cell energy needs, and it decreases the heart rate (negative chronotropic effect).
Atrial fibrillation
Atrial fibrillation is a type of arrhythmia where the heart’s upper chambers known as atria, don’t contract normally, but quiver due to a reentry phenomenon where a single electrical impulse activates cells several times so they are excited but they couldn’t fully contract, which leads to blood stagnation in atria. Those impulses may cause an increase in the rate of ventricular contractions. Digoxin reduces the electrical conductivity through the AV node, thus reduces the rate of ventricular contractions. Digoxin can be used along with beta-blockers or calcium channel blockers.
Supraventricular arrhythmias
Digoxin can be used in the treatment of other supraventricular arrhythmias besides atrial fibrillation, although atrial fibrillation represents the type of heart rhythm disorder that is most commonly treated by this drug. This drug reduces the electrical conductivity over the AV node, preserving the rhythm of the ventricles.
Cautions and contraindications of Digoxin
Like all other medications, digoxin shouldn’t be used in certain states and conditions as it could worsen them. Some important ones include AV block, WPW syndrome, sick sinus syndrome, ventricular fibrillation, low potassium ion levels, hypertrophic obstructive cardiomyopathy, renal failure, and acute myocardial infarction.
Sick sinus syndrome
Sick sinus syndrome includes heart rhythm disorders that are induced by irregular work of sinoatrial node, a natural pacemaker of the heart. In these conditions, the heart rhythm may become decreased, increased, or it represents a combination of these two. Digoxin should be avoided, as it could induce or worsen bradycardia, or cause a sinoatrial block.
Hypertrophic obstructive cardiomyopathy
Hypertrophic obstructive cardiomyopathy is a condition characterized by a thickened part of the heart with a limited ability to pump blood. Digoxin can worsen the obstruction of blood outflow due to its positive inotropic effects.
Acute myocardial infarction
A heart attack occurs when part of the heart is cut off from blood supply, leading to the death of heart cells. Due to digoxin’s inotropic effect, the need for energy may increase in heart muscle cells, causing ischemia, so its use is not recommended.
Low potassium levels in the blood
Hypokalemia (low potassium levels) may increase the chance of digoxin toxicity because digoxin blocks the Na+/K+-ATPase by binding to the same site as potassium, and when potassium levels are low, digoxin can easier bind to the Na+/K+-ATPase.
Renal failure
Renal failure (kidney failure) is a condition in which the kidneys lose their function, and their ability to eliminate toxic substances and waste from the organism decreases. Renal failure can lead to digoxin toxicity, as it is primarily eliminated by the kidneys and digoxin can cause kidney failure.
Ventricular fibrillation
Ventricular fibrillation is a life-threatening heart rhythm disorder that can lead to hemodynamic collapse, because ventricles quiver inefficiently, without pumping the blood into circulation. Digoxin is contraindicated in this condition, as its toxicity is associated with ventricular arrhythmia, worsening the condition and increasing the mortality rate.
AV block (atrioventricular block)
AV block is a condition where the conduction between the atria and ventricles of the heart is impaired. In second degree AV block some of the electrical impulses are unable to pass from the atria to the ventricles, and in third-degree AV block that conductivity is completely obstructed so the ventricles need to create a new abnormal rhythm, as known as escape rhythm. The heart rate in AV block is slow, and digoxin due to its effects on AV node can worsen those symptoms and should be avoided.
WPW syndrome (Wolff-Parkinson-White syndrome)
WPW syndrome represents an abnormal electrical pathway inside the heart, changing the heart rhythm. Bundle of Kent is an accessory pathway that connects the atria and ventricles, bypassing the atrioventricular node. This condition often doesn’t show any symptoms, but sometimes, the supraventricular tachycardia leads to dizziness, palpitations, and even fainting. As digoxin decreases the conductivity in the AV node, the Bundle of Kent pathway takes its role, and tachycardia is increased.
Side effects
Digoxin can express some side effect in certain people. Some of the important ones are:
- arrhythmia – arrhythmia is the most common and most dangerous side effect of digoxin; almost every type of arrhythmia is possible, even multiple abnormalities of heart rhythm in one patient; most common ones are periodical ventricular contractions, unifocal or multiform premature ventricular contractions (bigeminy or trigeminy); sinus bradycardia can occur, as well as AV block, and ventricular fibrillation
- hyperkalemia – high potassium levels in the blood that can lead to dangerous, life-threatening heart rhythm disorders; hyperkalemia can occur due to digoxin’s inhibition of Na+/K+-ATPase, so more potassium is found out of cells
- effects on the digestive system – anorexia, nausea, vomiting, diarrhea, upset stomach, and stomach pain can occur due to the central vagus nerve stimulation
- effects on central nervous – those side effects include headache, dizziness, confusion, anxiety, depression, hallucinations, as digoxin can pass through the blood-brain barrier
- gynaecomastia – enlargement of male breast tissue can happen possibly due to digoxin’s steroidal chemical structure
- visual problems – digoxin can lead to color vision deficiency called xanthopsia where a patient has a predominance of color yellow; blurred vision might occur, as well as seeing white or yellow halos around objects
Interactions of digoxin
Like all other medications, digoxin can come in interaction with other drugs so it’s important to tell your doctor or your pharmacist which medications are you taking. Some of the important ones include interactions with:
Diuretics
Diuretics, also known as water pills are part of the treatment of high blood pressure and heart failure. Thiazides and loop diuretics can cause hypokalemia, so digoxin toxicity may be worsened.
Calcium channel blockers
In severe cases of atrial fibrillation, a combination of calcium channel blockers and digoxin is sometimes used. Due to the inhibitory effect of calcium channel blockers on a protein responsible for the pumping of foreign substances out of cells, called P-glycoprotein, the levels of digoxin concentration may rise in blood so its concentration should be monitored, and the dose adjusted.
Aspirin
Aspirin is often used as an antiplatelet drug or pain killer. It can cause increased levels of digoxin in the blood leading to the expression of its toxic effects.
Amiodarone
Amiodarone is an antiarrhythmic drug that is used in the treatment of many abnormal heart rhythms. It can lead to an increase of digoxin levels in the blood, so it needs to be monitored and well-adjusted.
Beta blockers
Beta blockers are commonly prescribed drugs for various cardiovascular diseases, and they’re sometimes combined with digoxin in treatment of atrial fibrillation. Beta blockers may additionally reduce the electrical conductivity through the AV node.
Macrolide antibiotics
Macrolide antibiotics can lower the number of gut bacteria that metabolize digoxin, furthermore leading to increase in digoxin concentrations in blood, causing its toxic effects.
